Understanding Glaucoma: Types and Causes
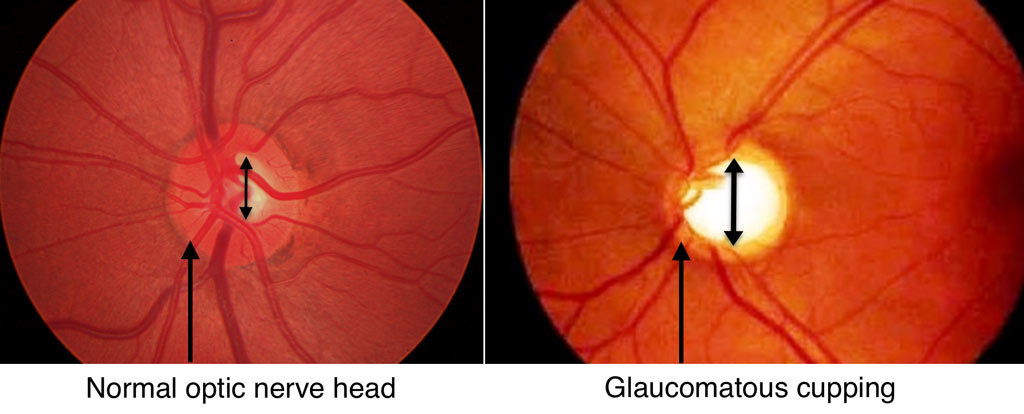
Glaucoma includes a group of diseases that damage the optic nerve and reduce visual field. Researchers have identified more than fifty causes. Doctors usually classify glaucoma by the eye’s drainage system, called the anterior chamber “angle.” Below, we highlight some of the most common types.
Types of Glaucoma
Primary Open-Angle Glaucoma
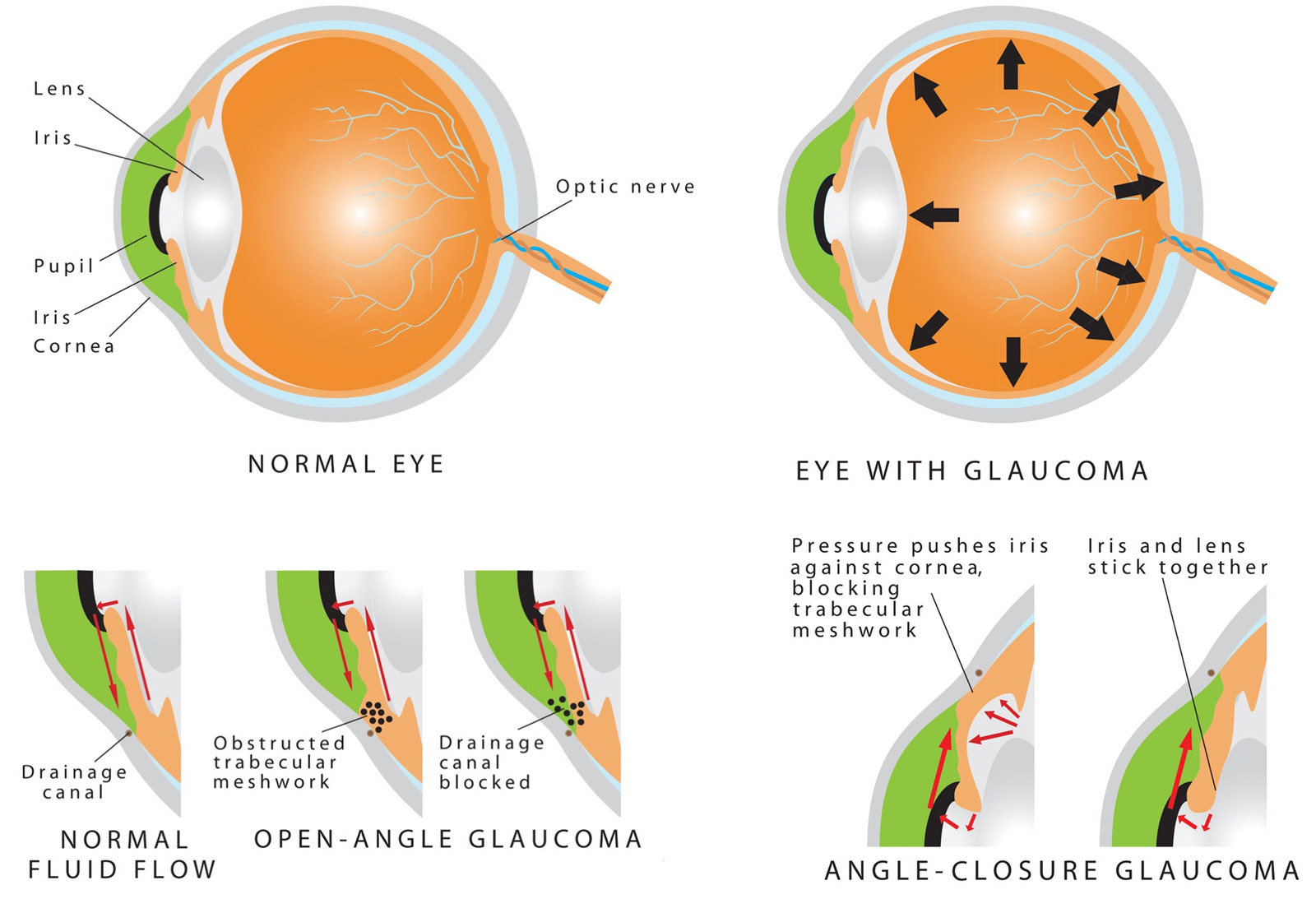
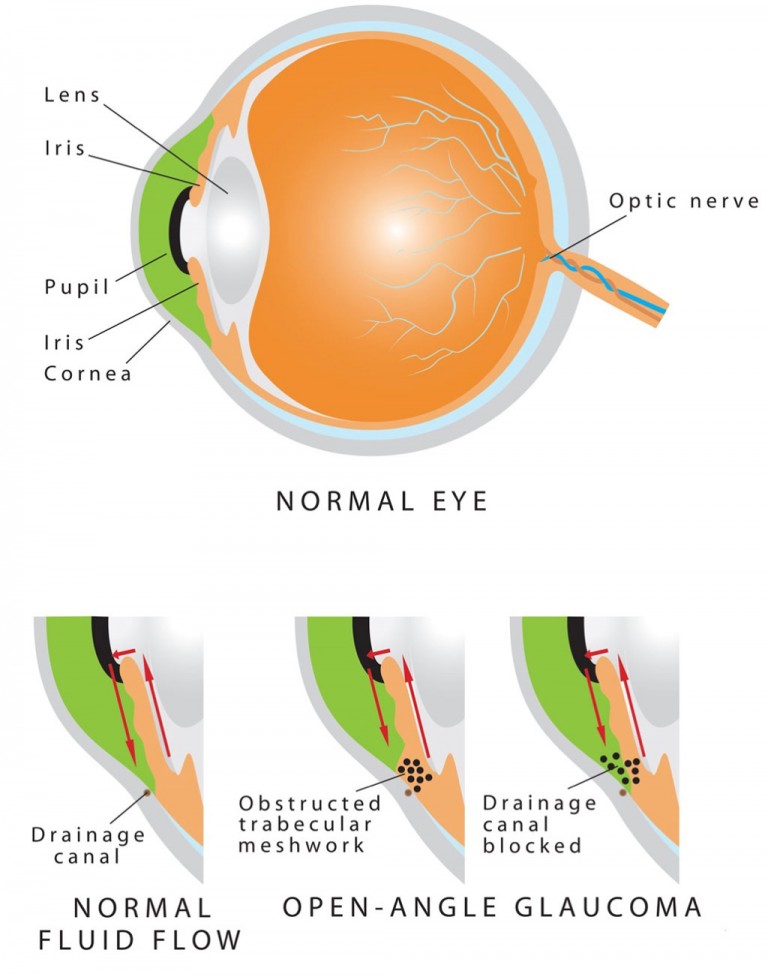
Primary Open-Angle Glaucoma (POAG), also called chronic open-angle glaucoma, is the most common type of glaucoma. It causes elevated intraocular pressure, optic nerve cupping and atrophy, and typical visual field defects. In “primary” glaucoma, no other eye or systemic disease causes the condition. Gonioscopy shows a normal anterior chamber angle.
POAG usually affects both eyes equally. In the U.S., 1.5%-2% of people have POAG, most often after age 40.
The exact cause is unknown, but several risk factors increase the likelihood. These include high intraocular pressure, age, African or Hispanic ancestry, thin corneas, and family history. Diabetes and myopia may also contribute. POAG affects both men and women equally.
Normal Tension Glaucoma (Low Tension Glaucoma)
Normal Tension Glaucoma (NTG), also called Low Tension Glaucoma (LTG), closely resembles Primary Open-Angle Glaucoma. The main difference is that NTG occurs without elevated intraocular pressure (above 21 mmHg).
Doctors treat NTG like other types of glaucoma by lowering eye pressure. Studies show that even when pressure is within the normal range, further reduction can slow optic nerve damage and prevent visual field loss.
Secondary Open-Angle Glaucoma
Secondary open-angle glaucoma resembles primary open-angle glaucoma in appearance. The anterior chamber angle remains open and visible, without obvious obstruction. However, an underlying eye or systemic condition increases resistance to fluid outflow and raises intraocular pressure.
Therefore, careful gonioscopy plays an important role. Although the angle appears open, subtle changes often provide clues that help ophthalmologists identify the cause.
Pseudoexfoliation Syndrome
Pseudoexfoliation syndrome can cause a form of open-angle glaucoma. Fibrillary material deposits on structures in the anterior chamber, including the iris, lens capsule, zonules, and trabecular meshwork. The condition may affect one or both eyes, and findings often differ between eyes.
Risk increases with age, especially after 50 and most commonly after 70. It also increases in women and people of Scandinavian descent. However, not all patients develop pseudoexfoliation glaucoma.
When material accumulates in the trabecular meshwork, it restricts fluid drainage and raises intraocular pressure. As a result, glaucoma may develop. Treatment focuses on lowering eye pressure using medications, lasers, or surgery.
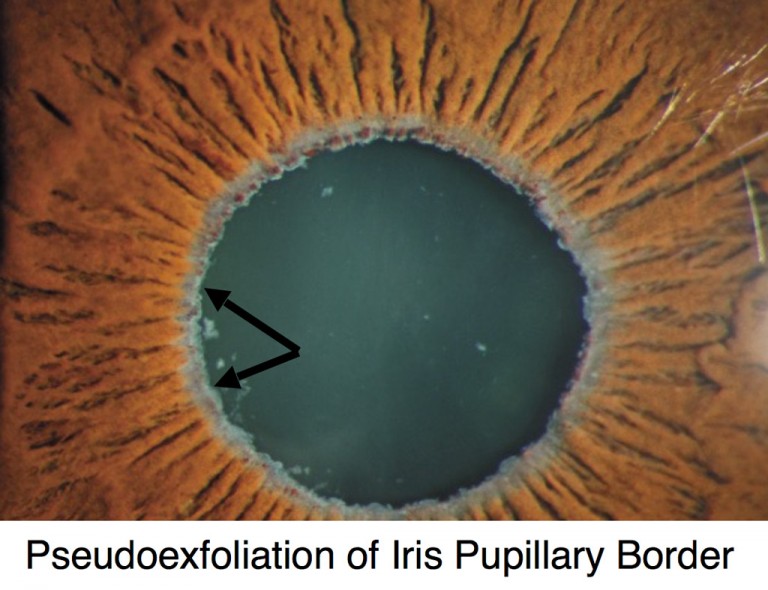
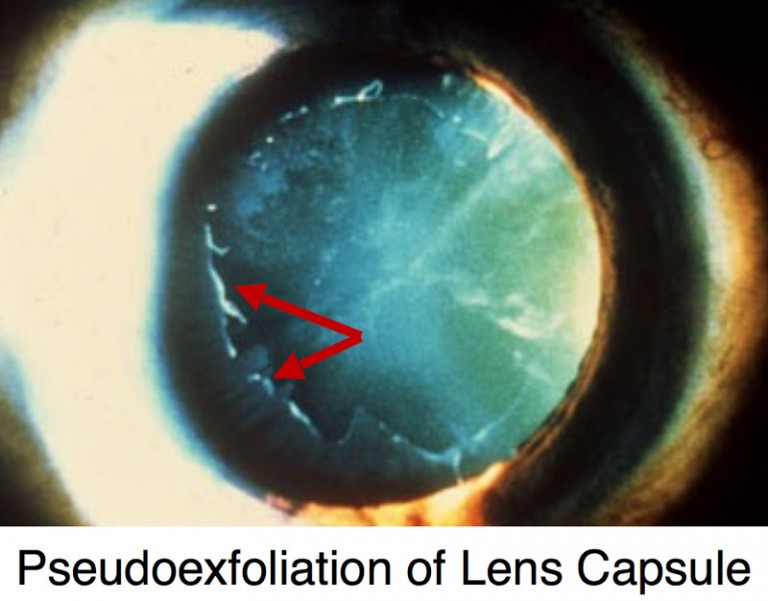
Iris Atrophy
Pseudoexfoliation syndrome also causes several additional eye findings. These include iris atrophy, a floppy iris (iridodonesis), poor pupil dilation, and zonular weakness with lens instability (phacodonesis).
As a result, cataract surgery can become more complex. These features can also trigger significant eye pressure spikes immediately after surgery. However, GAT doctors have extensive experience performing cataract surgery in patients with pseudoexfoliation syndrome and managing post-operative care effectively.
Pigment Dispersion Syndrome
Pigment Dispersion Syndrome occurs when pigment deposits on eye structures. These include the cornea (Krukenberg spindle), trabecular meshwork, and lens capsule (Zentmayer line). The condition also causes mid-peripheral iris transillumination defects and often a backward bowing of the iris.
Risk increases in Caucasian patients, men, and people with myopia. It usually appears between ages 20 and 50. However, not all patients develop pigmentary glaucoma.
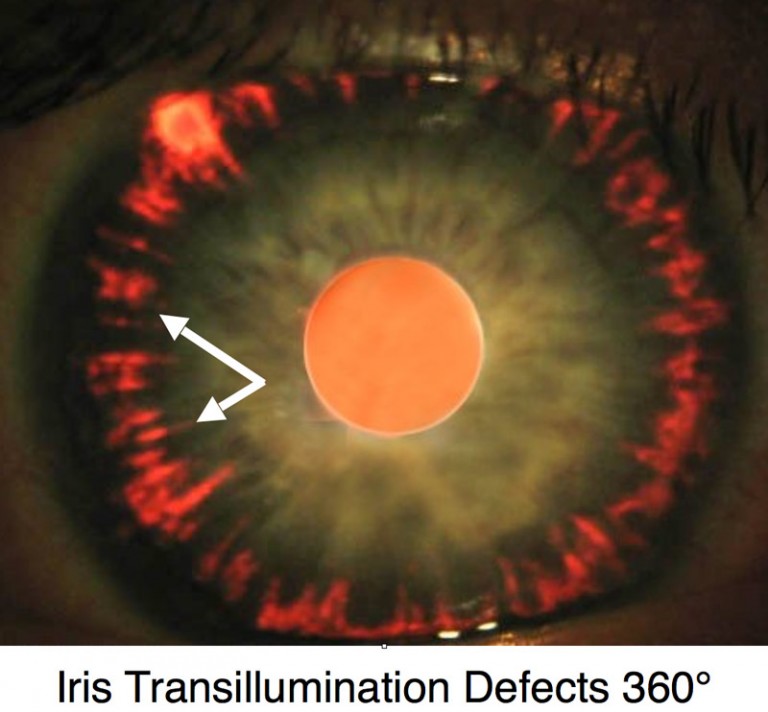
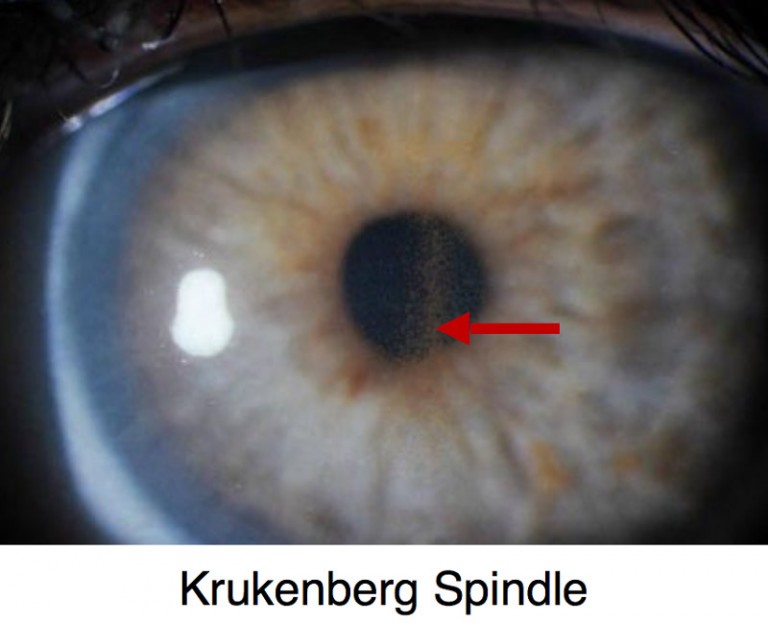
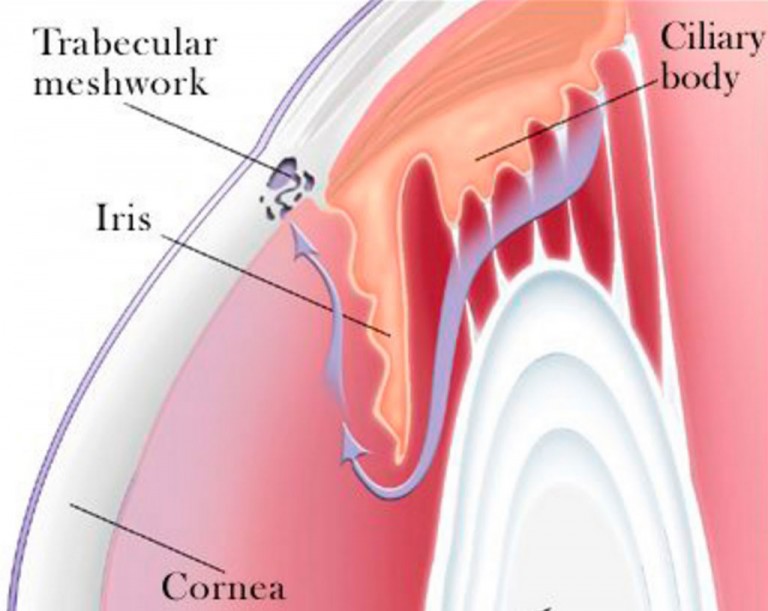
Trabecular Meshwork
On gonioscopy, doctors see heavy pigment in the trabecular meshwork. As pigment releases into the aqueous humor, eye pressure can fluctuate widely. This pigment can block fluid drainage and raise pressure.
Therefore, treatment focuses on lowering intraocular pressure. Options include medications, lasers, and surgery. Notably, patients often respond well to laser trabeculoplasty.
Steroid-Induced-Glaucoma
A number of medications, most notably corticosteroids (“steroids”), have been associated with elevation of intraocular pressure. Although topical steroid eye drops and intra/peri-ocular steroids (e.g. intravitreal, intracameral, subtenon, retroseptal) are most likely to cause pressure elevations, any form of steroids including oral, topical creams, nasal sprays, and injections can increase intraocular pressure. While prescription steroid medications are often more potent and more likely culprits, numerous over-the-counter creams and nasal sprays can also cause increased eye pressure.
It is estimated that ~30% of all people have a mild-moderate elevation (up to 11 mmHg rise from baseline) with use of ocular steroids (drops or injectable) and 5% have an elevation of greater than 15 mmHg usually requiring treatment. Among patients with preexisting glaucoma, the likelihood of a pressure elevation rises significantly.isting Glaucoma, The Likelihood Of A Pressure Elevation Rises Significantly.
More recently, it has been observed that patients receiving various multiple non-steroid intravitreal injections (e.g. bevacizumab/Avastin®, ranibizumab/Lucentis®, aflibercept/Eylea®) can also have sustained intraocular pressure rise. These medications are often used for retinal disease including macular degeneration, diabetes, and macular edema (swelling).
Treatment for steroid (medication) induced glaucoma is similar to other secondary open-angle glaucomas and medications are usually successful. Cases requiring surgical intervention also have a high degree of success.
Other examples of secondary open-angle glaucoma include:
- Inflammatory Glaucoma
- Intraocular Tumor-Induced Glaucoma
- Lens Induced Glaucoma (E.G. Phacolytic, Lens Particle, Phacoantigenic)
- Traumatic Glaucoma (E.G. Accidental, Surgical)
- Elevated Episcleral Venous Pressure (E.G. Sturge-Weber Syndrome, Arteriovenous Fistula, Thyroid-Associated Orbitopathy)
Acute Angle-Closure Glaucoma
Acute angle-closure glaucoma starts suddenly and is an eye emergency. If not treated quickly, it can cause permanent damage in hours to days. Patients often experience sudden eye pain, redness, and blurred vision. The pain usually centers over the brow. Nausea, vomiting, and sweating are common, which can sometimes lead to misdiagnosis in an emergency room.
Exam shows a very shallow front chamber, a cloudy cornea, and a mid-sized, fixed pupil. Gonioscopy reveals a closed angle with no visible drainage structures.
Treatment aims to stop the attack and lower eye pressure. Doctors first use eye drops and oral medicines. Pupil-constricting drops like pilocarpine may help break the attack. A laser iridotomy usually follows to prevent repeat attacks. The other eye often receives a laser iridotomy as a preventive measure.
Acute attacks can leave lasting effects. Vision may be affected, and recovery varies. The cornea may develop folds that usually resolve, though some cell loss can occur. Rarely, chronic corneal swelling develops, especially in patients with Fuch’s dystrophy or long-standing closure.
The iris can suffer from reduced blood flow, causing inflammation or tissue damage. This may lead to permanent pupil dilation, sectoral atrophy, or spiraling of iris fibers. Sudden high eye pressure can also cause lens opacities called glaukomflecken, which appear as small white spots under the front lens surface.
Chronic Angle-Closure Glaucoma
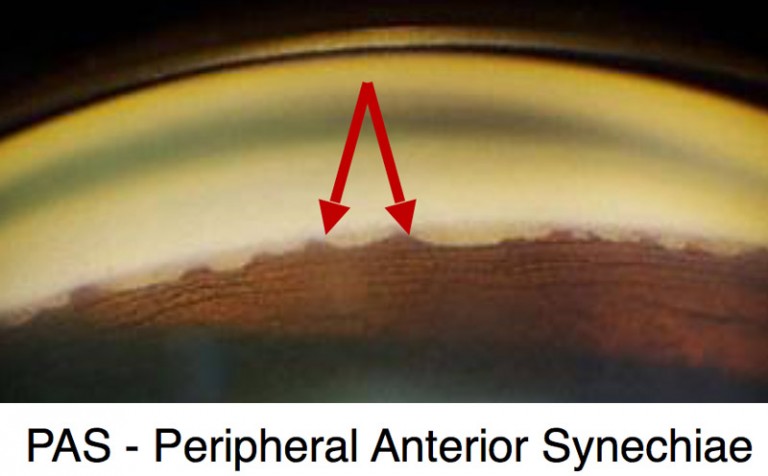
Chronic angle-closure glaucoma occurs when iris tissue blocks the anterior chamber angle without another eye or systemic cause. Over time, peripheral anterior synechiae form between the iris and trabecular meshwork. As a result, fluid drainage slows and eye pressure rises.
In many cases, pupillary block triggers this process. A block forms between the lens and the iris. Fluid then collects behind the iris and pushes it forward. Consequently, the angle closes and permanent scarring develops.
This condition often goes undiagnosed and may mimic open-angle glaucoma. Therefore, gonioscopy plays a critical role in diagnosis. Accurate evaluation requires full visualization of the angle. GAT doctors possess this expertise through specialized glaucoma fellowship training.
Treatment focuses on lowering intraocular pressure. In addition, doctors treat the pupillary block with laser iridotomy to slow or stop further angle damage. However, closure may continue even after treatment. For this reason, regular gonioscopy remains essential. Most patients respond to medications, although some require glaucoma surgery.
Secondary Angle-Closure Glaucoma
Similar to primary angle-closure glaucoma, patients with secondary open angle glaucoma have an anterior chamber angle which at least partly occluded, often permanently by peripheral anterior synechiae (PAS; scar tissue extending between the iris and the trabecular meshwork). However, in secondary angle-closure glaucoma, the occlusion of the angle is associated with an ocular or systemic cause. Careful gonioscopy often shows subtle changes that your ophthalmologist can detect to give clues as to the cause of the angle closure, a skill all GAT Doctors have as a result of their fellowship training in glaucoma.
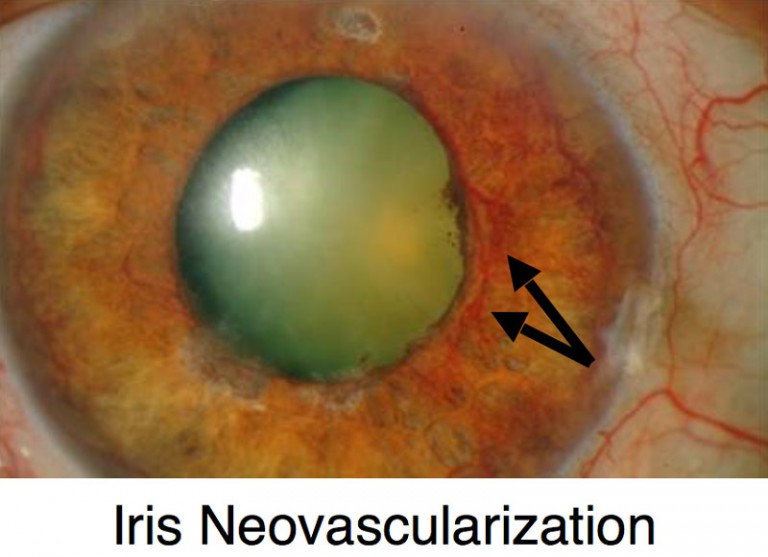
Iris Neovascularization
Neovascular glaucoma is a severe form of secondary angle-closure glaucoma. It develops when abnormal blood vessels grow in the iris and trabecular meshwork. These vessels cause bleeding, scarring, and peripheral anterior synechiae, which close the angle and raise eye pressure.
This condition results from other eye or systemic diseases. Most commonly, it occurs with diabetes, central retinal vein occlusion, or ocular ischemic syndrome. Other causes include chronic inflammation, trauma, tumors, radiation, and vascular disease.
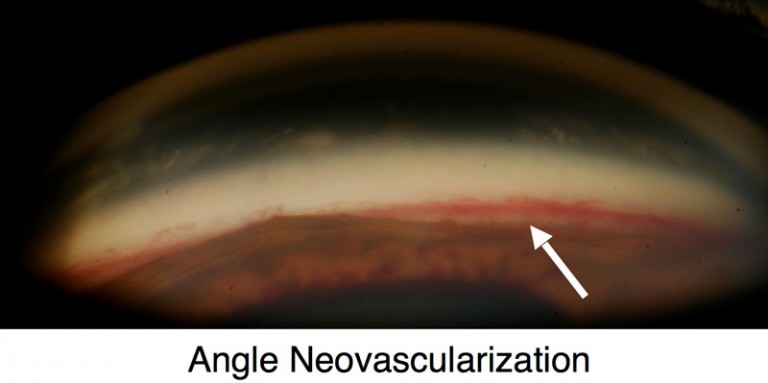
Angle Neovascularization
Patients often develop sudden vision loss, eye pain, redness, and very high intraocular pressure. Therefore, treatment focuses on two goals. Doctors must control eye pressure and treat the underlying disease. Medications alone often fail, so surgery is usually required, most often with a glaucoma drainage implant.
Blood vessels can appear in a normal angle during gonioscopy. Their visibility depends on iris color and angle width. They appear in over half of blue-eyed patients but in fewer than 10% of brown-eyed patients. They also appear more often in wide angles. Therefore, careful evaluation matters. GAT doctors perform gonioscopy on all patients and accurately distinguish normal from abnormal vessels.
Inflammatory Glaucoma
Ocular inflammation can cause many eye problems. These include elevated intraocular pressure, glaucoma, corneal disease, cataracts, retinal disease, and scarring of the conjunctiva, cornea, iris, anterior chamber angle, and retina.
Inflammatory glaucoma develops through several mechanisms. Over time, peripheral anterior synechiae and posterior synechiae form. These scars block fluid flow and raise eye pressure.
Therefore, treatment focuses first on the underlying inflammation. Doctors often use topical or oral steroids and other anti-inflammatory medications. In addition, they treat high eye pressure with glaucoma drugs. However, surgery often becomes necessary due to the aggressive nature of this condition.
Glaucoma Suspect (Borderline Glaucoma)
Patients who are deemed to be a glaucoma suspect (borderline glaucoma) may show some signs of glaucoma without definitive disease, or may carry risk factors for developing glaucoma. Often, patients are classified as “low risk” or “high risk” glaucoma suspects based on the number of findings or risk factors. Classically, patients described as a glaucoma suspect had one of the following:
- Visual field changes consistent with glaucoma
- Optic nerve or nerve fiber layer suspicious of glaucoma
- Intraocular pressure of greater than 21 mmHg
Several criteria have been associated with an increased risk of glaucoma. Patients may also be considered if they have some of the following:
- Level of Intraocular Pressure Rise
- Cup-to-disc Ratio (optic Nerve Appearance)
- Family History of Glaucoma
- Age
- Race
- Central Corneal Thickness
- Associated Diseases (e.g. Diabetes, Myopia)
Although there is no way to know which glaucoma suspects will ultimately develop glaucoma, your ophthalmologist will discuss your risk factors with you and follow your at regular intervals.
Narrow Angle and Plateau Iris Syndrome
Plateau Iris SyndromeWhile both a narrow angle and plateau iris can be associated with development of angle closure glaucoma, they are not synonymous with glaucoma. Rather, both a narrow angle and plateau iris are anatomic descriptions of the anterior chamber angle between the cornea and iris.
Narrow Angle
A narrow anterior chamber angle increases the risk of acute and chronic angle-closure glaucoma. Although studies attempt to predict who will develop glaucoma, none provide consistent results. Therefore, not all patients require treatment.
However, doctors recommend laser iridotomy for patients with elevated intraocular pressure, peripheral anterior synechiae, appositional angles, prior angle closure, family history, or symptoms of intermittent angle closure. Regardless of treatment, patients should recognize warning signs. These include eye pain, redness, blurred vision, colored halos, headache, nausea, and vomiting.
Additionally, some medications raise the risk of acute angle closure. These include cold and allergy drugs, urological medications, and antidepressants. Therefore, patients should inform their ophthalmologist about regular use, as it may affect treatment decisions.
Plateau Iris Syndrome
Plateau iris syndrome has a normal-depth front chamber in the center of the eye with a flat iris. However, an eye exam called gonioscopy shows a narrow drainage angle. Doctors often confuse it with pupillary block, especially in younger patients with nearsightedness who have sudden angle-closure attacks.
Although the causes differ, treatment starts with a laser iridotomy. This procedure may open the angle slightly. However, the angle stays narrow even after the laser creates an opening in the iris. Because of this, doctors often diagnose plateau iris during an angle-closure attack that happens after iridotomy.
The condition develops because the outer part of the iris and the ciliary body sit too far forward. When the pupil enlarges, these structures block the eye’s drainage system. As a result, treatment may include close follow-up, pupil-constricting eye drops, laser iridoplasty, or lens or cataract removal.
Childhood Glaucoma (Congenital Glaucoma)
Childhood glaucomas encompass both primary congenital glaucoma (also called pediatric or infantile glaucoma) as well as juvenile glaucoma which may be diagnosed after age 3 and into early adulthood. Please refer to Childhood (Congenital) Glaucoma page for more information.
 DONATE NOW
DONATE NOW