What is a Trabeculectomy?
When eye drops, pills, or laser surgery fail to lower intraocular pressure to a safe level, your ophthalmologist may recommend glaucoma surgery. Surgeons reduce pressure in a glaucoma eye by creating a new drain, a procedure called trabeculectomy.
During this operation, the surgeon removes a tiny piece of the eye wall, which may include the trabecular meshwork (the natural drain). This removal opens a new drain, creating a bypass for the trabecular meshwork and lowering eye pressure. Fluid now drains more easily through the new opening into a reservoir (bleb) beneath the conjunctiva, and the body absorbs the fluid.
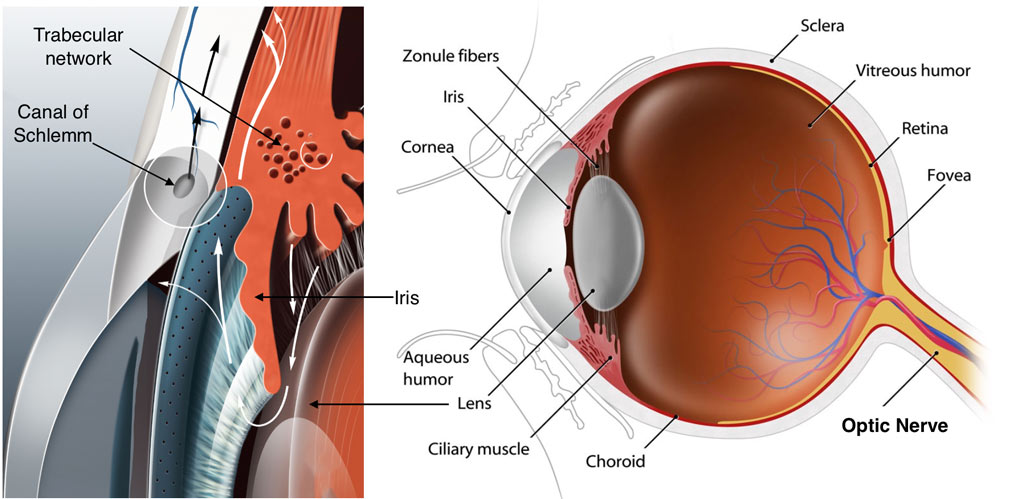
Newly Made Drain
The natural response of the body is to heal this newly made drain as it does with every other wound or injury the body sustains. However trabeculectomy surgery is unique in that we need the drain to remain open so that the eye pressure remains controlled. At the same time we need the surface tissues (conjunctiva) to heal back down so that the internal fluid of the eye does not leak into the tear film (bleb leak), as that could be a risk for infection. The risk of scarring down the drain and failure of the procedure is higher in younger individuals (less than 40 yrs), patients of African-American ancestry, history of previous eye surgery, previous ocular inflammation (uveitis) and in patients with neovascular glaucoma.
When your doctor performs a trabeculectomy procedure, they will often apply an anti-scarring medicine called Mitomycin (MMC) or 5-Flurouracil (5FU) to the surface tissues of your eye to reduce the chance of surgical failure. Adjuvant use of these drugs with trabeculectomy surgery has vastly improved the success rate of the procedure. Sometimes even with use of these drugs in surgery your eye might exhibit an exuberant healing response. In these cases your doctor might elect to inject 5-Flurouracil during your postoperative visits to help slow down the healing response.
What is My Chance of Success With a Trabeculectomy?
Although the results of the trabeculectomy depend on numerous factors and can vary greatly, as a general rule approximately 70% of operated eyes will have satisfactory eye pressure and no need for medication one year after surgery. If doctors add eye drops, over 90% of eyes achieve satisfactory lowering of eye pressure.
The goal of a trabeculectomy is to lower eye pressure. Lowering eye pressure helps protect the operated eye from further glaucoma damage and preserves its vision. Although vision sometimes can improve following trabeculectomy, in most eyes it remains unchanged. Occasionally, there can be loss of vision. Sometimes your doctor will combine the trabeculectomy surgery with cataract surgery. In these cases there may be some visual improvement from clearing of the cataract and replacing it with a clear intraocular lens implant.
What Steps Does a Surgeon Take During a Trabeculectomy Procedure?
After you and your doctor decide to proceed with trabeculectomy, you will meet with our preoperative scheduling nurse.
The nurse will provide detailed instructions on how to prepare for surgery and arrive at the operating room. See Preoperative instructions for more information.
Surgeons perform trabeculectomy as an outpatient procedure in an ambulatory surgery center. The surgery usually takes less than one hour. They typically use local anesthesia with intravenous sedation. An injection of local anesthetic through the eyelid numbs the eye completely, preventing movement and discomfort during surgery. Sometimes, they use general anesthesia, putting the patient to sleep. Local anesthesia offers several advantages: it causes less pain after surgery, avoids sore throat from the airway tube, and allows patients to regain alertness quickly without nausea. Local anesthesia also carries less risk than general anesthesia, especially for elderly patients or those with health problems.
Postoperative Monitoring and Recovery
After a trabeculectomy, your ophthalmologist usually covers the eye with a patch and protects it with a plastic shield overnight. The next morning, your ophthalmologist removes the patch and examines the eye. They then prescribe eye drops to relax the eye muscles, prevent infection, and reduce inflammation. Occasionally, they may also prescribe a pill to further reduce inflammation. Following your ophthalmologist’s instructions is important, as proper use of these medications can greatly affect the success of the procedure. See Postoperative Instructions.
For several weeks following the surgery, your ophthalmologist will observe your eye closely and examine you frequently. Because it is not possible to know the precise size of the opening to make in the eye to drain fluid, sometimes too much fluid may drain after surgery. Also it is not possible to predict your individual healing response to the surgery. If your eye pressure is running higher than intended, your doctor may use a laser during your postoperative visits to cut the sutures laying the trap door down to promote further flow of fluid from within the eye. It may take up to 12 weeks after your surgery for the healing to be complete. During this time it is not unusual for your intraocular pressure, as well as vision to fluctuate. You will be ready to change your glasses prescription at around 6-8 weeks after surgery.
ExPRESS® Glaucoma Mini Shunt
In a traditional trabeculectomy, the surgeon creates a new drain by punching a sclerostomy under a partial-thickness scleral flap. The size of this sclerostomy can be variable leading to an unpredictable intraocular pressure response in the early postoperative period.
The ExPRESS® Glaucoma mini shunt is a less than 3 mm long stainless steel implant that is inserted under a scleral flap, through a 27G needle track, to create a new drain. It diverts aqueous humor into the subconjunctival space through a standardized channel reducing intraocular pressure. The shunt has an inbuilt resistor that creates a standardized opening of 50 microns or 200 microns depending on the model implanted (P50, R50, P200). The entire procedure maintains a safer closed system, reducing the risk of anterior chamber collapse and vitreous shifting. Testing in magnetic fields up to 3 tesla confirms that the implant is completely MRI safe.
When a decision is made for glaucoma surgery, your doctor will discuss your options with you and if appropriate will discuss implantation of the ExPRESS® glaucoma mini shunt. The procedure for implantation of this shunt device is very similar to a trabeculectomy procedure. Surgeons most often use anti-scarring medications such as Mitomycin C or 5-Fluorouracil during surgery to reduce postoperative scarring. Refer to the trabeculectomy page for more details on what to expect if you are scheduled for this procedure.
 DONATE NOW
DONATE NOW