What is Cataract Surgery?
Cataract surgery and glaucoma surgery might be recommended by your doctor for treatment of your glaucoma. The management approach in the patient who has both glaucoma and cataract must be in many ways totally different from that of a person with cataract uncomplicated by glaucoma. Surgical techniques for both diseases have improved greatly and surgeons with up-to-date expertise in both subspecialties can provide superior outcomes for their patients. The doctors at Glaucoma Associates of Texas are expert cataract surgeons, with particular expertise in complex cataract surgery in glaucoma patients.
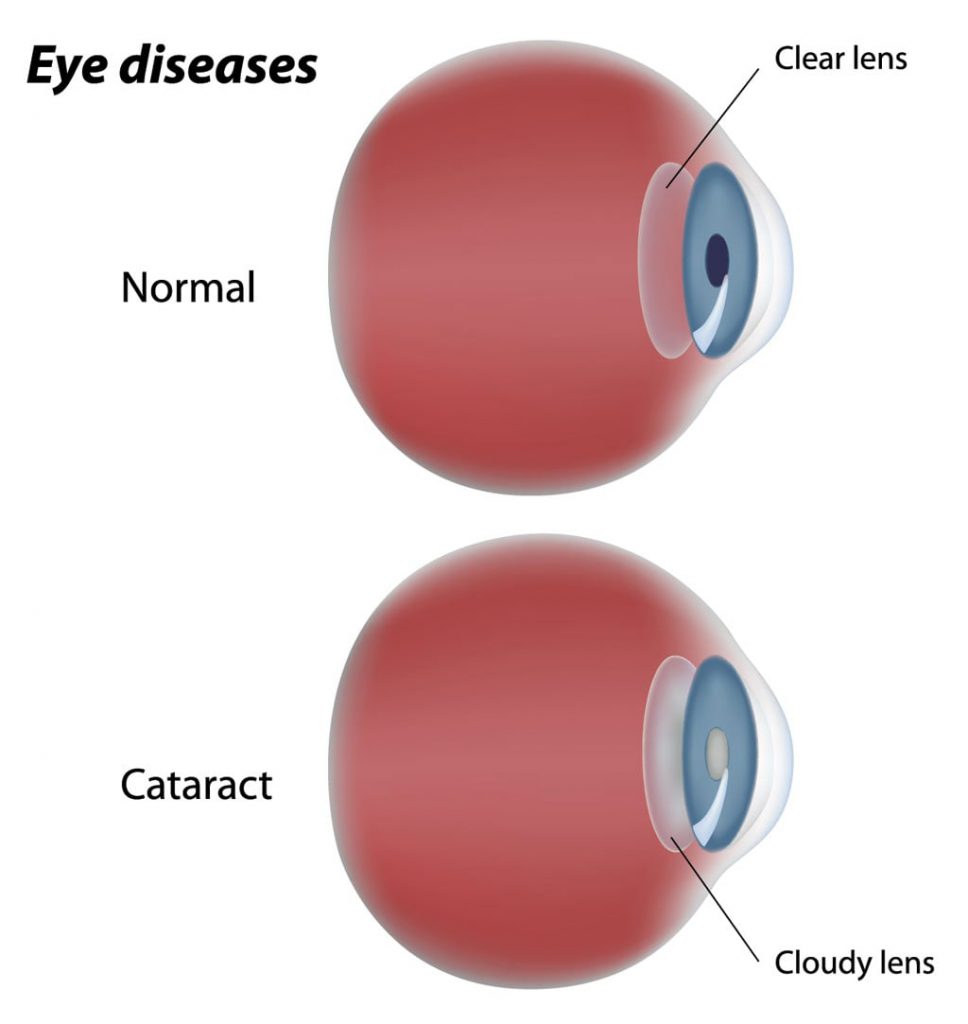
What is a Cataract?
A cataract is hardening and clouding of the natural crystalline lens within your eyeball. It is a normal process of aging. However, this process can occur sooner in glaucoma patients secondary to chronic use of glaucoma drops or from previous glaucoma surgery. In an eye with a narrow angle, a cataract further narrows the angle recess. In such eyes removal of the cataract alone will widen the anterior chamber angle and help prevent an acute angle closure attack.
Your doctor might recommend cataract surgery for treatment of your glaucoma and improvement of your vision. Often this may be combined with a glaucoma procedure as well, such as a GATT, trabeculectomy, glaucoma drainage implant, or others.
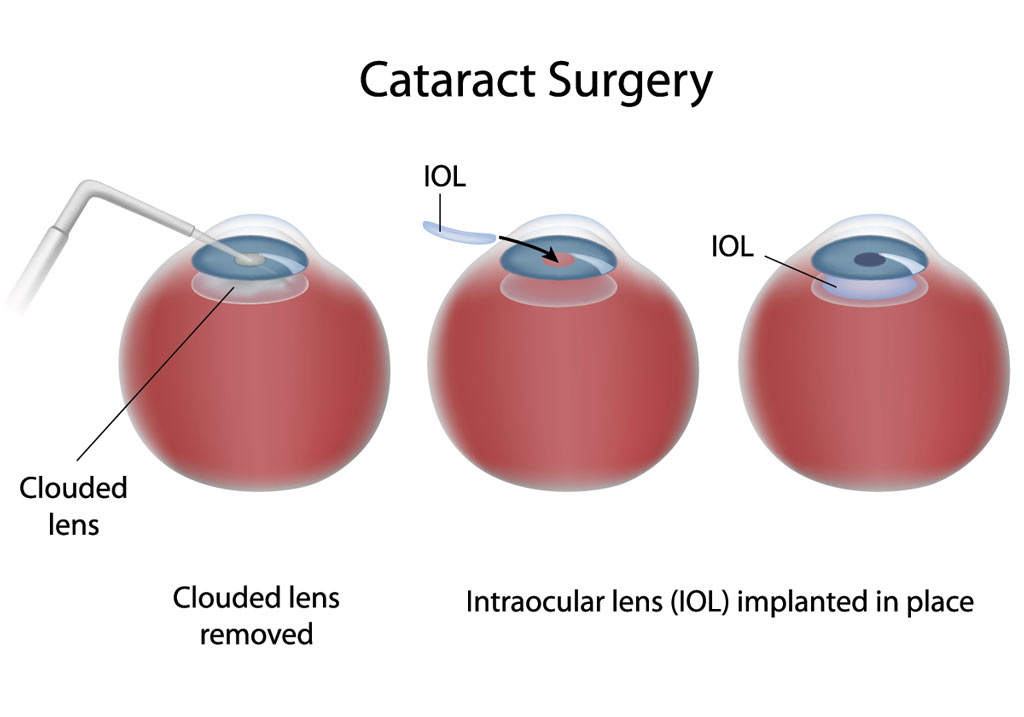
What is Cataract Surgery?
Removal of the cataract is a surgical procedure. Modern day cataract surgery is small incision and often sutureless. A tiny incision is made in the clear part of your eye called the cornea. A circular opening is made in the bag (capsule) which holds the cataract. A probe is inserted into your eye through this incision. The cataract is broken up into several tiny pieces with the help of an ultrasound probe and the cataract debris is removed using an automated irrigation-aspiration system. Once all the lens material is cleaned out, an intraocular lens implant (IOL) is placed into the bag. The artificial lens implant is placed in the natural anatomic position and it stays there for life. If the capsular bag is unstable (which is more common is some glaucoma patients), your doctor may chose to implant the IOL in a different position felt to be safer. On completion of the procedure, your doctor may place a stitch through your corneal wound, particularly if it combined with a glaucoma procedure; this stitch is easily removed in the clinic without any discomfort.
What Are My Lens Implant Choices?
In preparation for cataract surgery, certain measurements are taken of your eye to determine the correct power of the IOL to be placed in your eye at the time of cataract surgery. The axial length of the eyeball along with the corneal curvature is measured. Based on the measurements, various IOL choices will be presented to you. In general, there are 3 types of IOL choices:
- Monofocal lens implant: This is the “standard” lens that is covered by insurance without additional cost to the patient. It has the ability to correct your vision at distance (most commonly preferred by patients) or near, but not both. Often, reading glasses are needed for up-close vision. This lens is not able to correct astigmatism.
- Toric lens implant: This lens is able to decrease or eliminate your astigmatism (astigmatism causes distortion of vision if not corrected). However, similar to a “standard” lens above, it cannot correct both distance and near vision, and most patients will require reading glasses for up-close vision.
- Multifocal lens implant: This lens has the ability to improve BOTH your distance and near vision, decreasing and possibly eliminating the need for glasses.
Depending on the measurements completed prior to surgery, one or more of these IOLs may be options. Your doctor will discuss these options with you prior to surgery.
What is involved with Cataract Surgery?
When you and your doctor make a decision to proceed with Cataract surgery alone or in combination with a glaucoma procedure, you will meet with our preoperative scheduling nurse who will give you detailed instructions on how to prepare yourself for your upcoming surgery. See Preoperative Instructions for more information.
The surgery is an outpatient procedure performed in an ambulatory surgery center. The surgery itself takes about 30 minutes in most cases. The surgery can be done with drops or under local anesthesia with intravenous sedation. Rarely a general anesthetic is used, in which the patient is put to sleep for the operation. Local anesthesia offers several advantages over general anesthesia: local anesthesia is less risky than general anesthesia, especially in elderly patients or patients with other health problems; there may be less pain after surgery; there is no sore throat from the airway tube used in general anesthesia; and patients quickly return to normal alertness without the nausea often felt after general anesthesia.
After surgery, the eye generally is covered by an eye patch and protected by a plastic shield overnight. When you have surgery under topical anesthesia (anesthetic drops or gel), your doctor may only place a plastic shield over your eye and instruct you to start eye drops right away. On the morning following the surgery, the eye patch is removed and the eye is examined by your ophthalmologist. Eye drops are then started to prevent infection and reduce inflammation. It is important to take these as directed by your doctor since they can make a great deal of difference in the success of the procedure. See Postoperative Instructions for more details.
It takes about 4 to 6 weeks after cataract surgery for the vision to stabilize. You will be ready to change your glasses prescription (if needed) at that time.
 DONATE NOW
DONATE NOW