What is a Trabeculectomy?
When treatment with eye drops, pills, or laser surgery does not lower intraocular pressure to a safe level, your ophthalmologist may determine that glaucoma surgery should be performed. One way to reduce pressure in an eye with glaucoma is to make a new drain in the eye. This type of surgery is called a trabeculectomy.
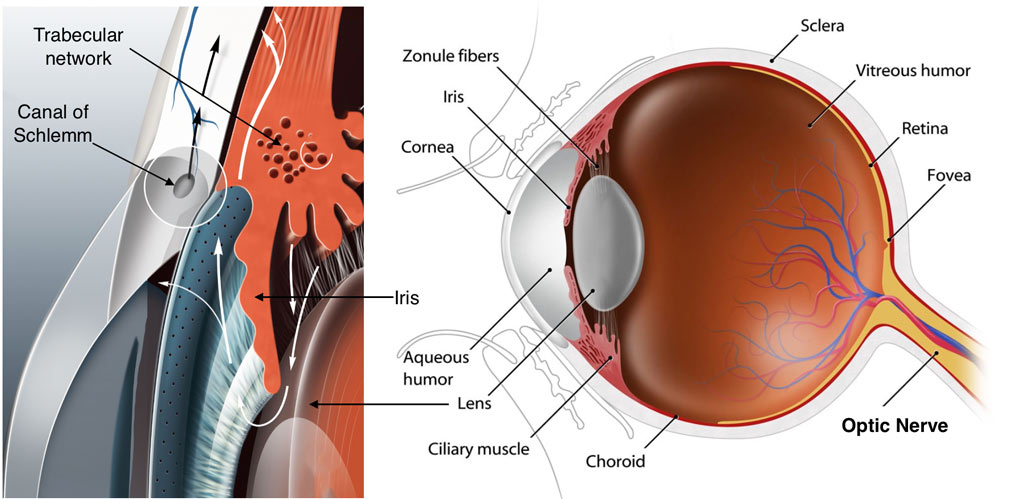
During this operation, a tiny piece of the wall of the eye, which may include the trabecular meshwork (the natural drain), is removed by the surgeon. This opens a new drain which creates a bypass for the trabecular meshwork to reduce eye pressure. The eye pressure is reduced because fluid can now drain with relative ease through the new opening into a reservoir (bleb) underneath the conjunctiva (which comprises the surface of the eye). The fluid is then absorbed by the body.
The natural response of the body is to heal this newly made drain as it does with every other wound or injury the body sustains. However trabeculectomy surgery is unique in that we need the drain to remain open so that the eye pressure remains controlled. At the same time we need the surface tissues (conjunctiva) to heal back down so that the internal fluid of the eye does not leak into the tear film (bleb leak), as that could be a risk for infection. The risk of scarring down the drain and failure of the procedure is higher in younger individuals (less than 40 yrs), patients of African-American ancestry, history of previous eye surgery, previous ocular inflammation (uveitis) and in patients with neovascular glaucoma. When your doctor performs a trabeculectomy procedure, they will often apply an anti-scarring medicine called Mitomycin (MMC) or 5-Flurouracil (5FU) to the surface tissues of your eye to reduce the chance of surgical failure. Adjuvant use of these drugs with trabeculectomy surgery has vastly improved the success rate of the procedure. Sometimes even with use of these drugs in surgery your eye might exhibit an exuberant healing response. In these cases your doctor might elect to inject 5-Flurouracil during your postoperative visits to help slow down the healing response.
What is my chance of success with a trabeculectomy?
Although the results of the trabeculectomy depend on numerous factors and can vary greatly, as a general rule approximately 70% of operated eyes will have satisfactory eye pressure and no need for medication one year after surgery. If eye drops are added, over 90% of eyes will have a satisfactory lowering of eye pressure.
The goal of a trabeculectomy is to lower eye pressure. By lowering eye pressure, it is hoped that the operated eye will be spared further glaucoma damage and can maintain its vision. Although vision sometimes can improve following trabeculectomy, in most eyes it remains unchanged. Occasionally, there can be loss of vision. Sometimes your doctor will combine the trabeculectomy surgery with cataract surgery. In these cases there may be some visual improvement from clearing of the cataract and replacing it with a clear intraocular lens implant.
What is involved with a trabeculectomy procedure?
When you and your doctor make a decision to proceed with the trabeculectomy surgery you will meet with our preoperative scheduling nurse who will give you detailed instructions on how to prepare yourself for your upcoming surgery and what is involved in getting to the operative room for the procedure. See Preoperative instructions for more information.
Trabeculectomy is an outpatient procedure performed in an ambulatory surgery center. The surgery itself takes less than one hour in most cases. The surgery is usually done under local anesthesia with intravenous sedation. An injection of local anesthetic through the eyelid numbs the eye completely so that it will not move during surgery, and there is no discomfort. Sometimes a general anesthetic is used, in which the patient is put to sleep for the operation. Local anesthesia offers several advantages. There may be less pain after surgery, and there is no sore throat from the airway tube used in general anesthesia. Patients quickly return to normal alertness without the nausea often felt after general anesthesia. With local anesthesia, there is less risk than with a general anesthetic, especially in the elderly or those with health problems.
After a trabeculectomy, the eye generally is covered by an eye patch and protected by a plastic shield overnight. On the morning following the surgery, it is removed and the eye is examined by your ophthalmologist. Eye drops are then prescribed to relax the muscles in the eye, prevent infection, and reduce inflammation. Occasionally, a pill may be prescribed, as well, to further reduce inflammation. It is important to take these as directed by your ophthalmologist since they can make a great deal of difference in the success of the procedure. See Postoperative instructions.
For several weeks following the surgery, your ophthalmologist will observe your eye closely and examine you frequently. Because it is not possible to know the precise size of the opening to make in the eye to drain fluid, sometimes too much fluid may drain after surgery. Also it is not possible to predict your individual healing response to the surgery. If your eye pressure is running higher than intended, your doctor may use a laser during your postoperative visits to cut the sutures laying the trap door down to promote further flow of fluid from within the eye. It may take up to 12 weeks after your surgery for the healing to be complete. During this time it is not unusual for your intraocular pressure, as well as vision to fluctuate. You will be ready to change your glasses prescription at around 6-8 weeks after surgery.
ExPRESS® Glaucoma Mini Shunt
In a traditional trabeculectomy procedure a new drain is created by punching a sclerostomy under a partial thickness scleral flap. The size of this sclerostomy can be variable leading to an unpredictable intraocular pressure response in the early postoperative period.
The ExPRESS® Glaucoma mini shunt is a less than 3 mm long stainless steel implant that is inserted under a scleral flap, through a 27G needle track, to create a new drain. It diverts aqueous humor into the subconjunctival space through a standardized channel reducing intraocular pressure. The shunt has an inbuilt resistor that creates a standardized opening of 50 microns or 200 microns depending on the model implanted (P50, R50, P200). The entire procedure is a safer closed system reducing the risk of anterior chamber collapse and vitreous shifting. The implant is completely MRI safe and has been tested in magnetic fields of up to 3 tessa forces.
When a decision is made for glaucoma surgery, your doctor will discuss your options with you and if appropriate will discuss implantation of the ExPRESS® glaucoma mini shunt. The procedure for implantation of this shunt device is very similar to a trabeculectomy procedure. Most often anti-scarring medications such as Mitomycin C or 5-Flurouracil will be used during surgery to reduce the chance of postoperative scarring. Please refer to the trabeculectomy page for more details on what to expect if you are scheduled for this procedure.
 DONATE NOW
DONATE NOW